Lower back pain is an increasingly common injury and complaint, with yearly numbers on the rise. In 2014-2015 1 in 6 Australians had complained about back pain (that is around 3.7 million people), as of 2018 that number had increased to 4 million (Australian Bureau of Statistics (ABS) 2017–18 National Health Survey (NHS))
But what are the causes? and more importantly what can you do to fix your back pain and build a lower back that is strong, robust and stays pain free?
This article will provide you with a overview of the most common mechanical causes of lower back pain, including disc bulges, herniations, sciatica, end plate fractures, stenosis, spondylosis, spondylolisthesis, and and muscular imbalance.
In no way is this an exhaustive list of all types of injury, but it covers the majority of the most common causes of lower back pain and injury.
This is a long overview article and the table of contents below allows you to navigate to the sections you will find the most useful.
Brian’s Note: There is common theory that back pain can be classed as “Non-Specific Lower Back Pain” or “NSLBP”. The problem with this approach is that it reduces the understanding the causes of back pain as to be all the same and somewhat vague in nature.
In reality, lower back pain should be viewed as a collection of different, specific issues; each with their own unique characteristics, challenges, solutions and contra-indications for treatment approaches.
Table of Contents
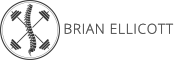
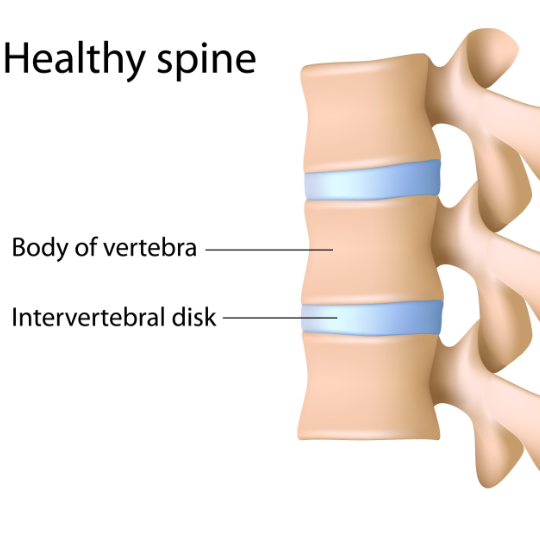
Basic Spinal Disc Anatomy
What Causes a Posterior Disc Bulge?
Disc bulges are a very common cause of lower back pain, although it should be noted that not all people with back pain have disc bulges; and conversely not all people with disc bulges have lower back pain.
Disc bulges occur when the outer layer of the disc, the annulus fibrosus weakens, and the inner material (from the nucleus pulposus) protrudes outward.
The most common cause of posterior disc bulges is repeated compressed flexion, which over 100’s of cycles will cause the bulge to form due to the hydraulic behaviour of the fluid inside the nucleus that delaminates the tough, collagen fibres of the annulus and drives the contents out towards the rear of the disc.

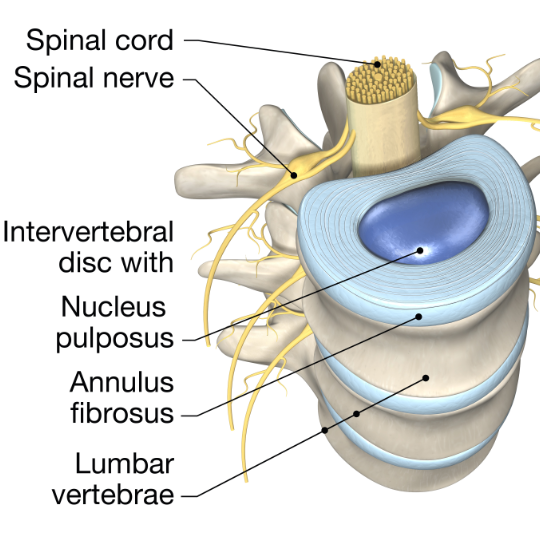
Brian’s Note: A basic visual example for mechanism behind damage from excessive flexion would be to imagine squashing the front end of a balloon; so that the air inside is forced to the rear, causing the rear end to “bulge”.
Although our discs are not quite as feeble as a balloon, and this process would take hundred’s if not 1000’s of repeated cycles of compressed flexion (forward rounding of the spine) to delaminate the the tough, collagenous fibres of the annulus fibrosus.
The amount of cycles needed is also dependant upon the compressive load paired with the flexion; think of technique breakdown on a 200kg deadlift for multiple reps versus sitting in a chair for hours with lumbar flexion.

Something to also note, that due to genetic differences in both anatomy (heavy and thick structure versus thin and light) and disc shape (ovoid vs. limacon or symmetrical vs. asymmetrical), there can be a great difference in one person’s tolerance to compressed flexion cycles versus another.
Flexion Movement vs. Flexion Moment
We must also differentiate lumbar flexion movement from lumbar flexion moment. Flexion movement requires the actual movement of the spine into a rounded position and of course the subsequent movement back to neutral or extension.
Flexion moment requires the creation of flexion torque, regardless of whether the spine moves or not. Imagine pushing a heavy load forwards, this would require the anterior muscle activation – but not a movement into flexion. This distinction is very important, as it lets understand how we can train and develop saggittal plane stability in the core and spine without the risk of delaminating the vertebral discs.
A good example of two different exercises that act on these two principles are a traditional sit-up (or abdominal crunch) versus a McGill Curl-Up.
In a traditional sit-up/curl we contract the abdominal muscles by rounding the lumbar spine into flexion and then relaxing, this gives us spinal movement. Yes we are strengthening our abdominal muscles to build strength, but at the expense of taking our lumbar discs though extra cycles of flexion.

In a McGill curl-up we strengthen our abdominal brace via flexion moment, we create a strong, challenging contraction in a way that does not sacrifice spinal position and integrity. In fact it begins building our skill to “brace”, which will transfer being able to lift, heavy awkward loads with a safer posture later in our rehabilitation.

“Flexion movement of the spine strains the layers of collagen in the spinal discs. When loads on the spine are small, movement is healthy. We often recommend the catâ€camel motion exercise taking the spine through an unloaded range of motion. Thus, there is a time and place for flexion motion. When the spine loads are high in magnitude with repeated flexion motion, the collagen fibres delaminate in a cumulative fashion. Slowly the nucleus of the disc will work through the delaminations and create a disc bulge.” – Professor Stuart McGill
What are the Causes of Disc Herniations?
Disc herniations occur when the outer layer of the disc ruptures, and the inner material protrudes outward, which can compress the spinal nerves. The most common cause of posterior disc herniations is compressed flexion, whereby the mechanics that created a disc bulge have not been addressed and the bulge has now progressed into a full blown herniation.

In the case of posterior disc herniations (which are the most common type and also often associated with sciatic like pain), the same mechanics of excessive compressed flexion have been present. The difference here is that bulge has now progressed by breaking through the last layer of the annulus, allowing the contents of the nucleus pulposus to leak outwards.

Brian’s Note: A simple visual example here would be to squeeze the front end of a jelly/jam doughnut, forcing the contents out of the rear of the doughnut.

Can Disc Bulges and Herniations Heal?
Yes…But it depends upon the correct identification and removal of the movement patterns and posture habits that have lead to their creation.
Although in some cases, surgery still may be required to fully heal the issue. This could be a procedure such as a disc discectomy, whereby the offending disc material is removed to relieve pressure on the nerve root or spinal cord. In general, non-surgical interventions are sought and exhausted first.
We must think of our aggravating movement habits as “picking at the scab”; if we don’t remove them, how will it ever get a chance to heal? In the case of posterior disc bulges and herniations, this means the reducing and managing the amount of flexion the lumbar spine is subject to, and keeping it well within the tolerable limits for that particular person.

Those familiar with the work of Dr. Robin McKenzie (The McKenize Method, Treat Your Own Back) will be aware of using positions (such as the Floppy Push-up/Prone Cobra/McKenzie press-up) that use end-range lumbar extension (the opposite movement to lumbar flexion) to encourage the protruding material of the nucleus back into the disc.

The cobra pose can be an extremely useful tool for some with disc bulges, but can also be absolute poison for others.
But why?
As with any exercise, method or treatment we must always be aware of it’s contra-indications (reasons when not to use it) first. While end-range extension can help a disc bulge/herniation caused by flexion, we must also be aware of its affects on other structures in the lumbar spine.
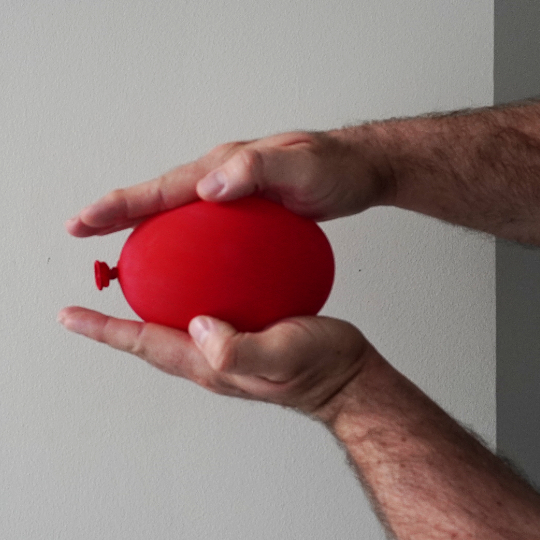
For example, if a person has lost significant disc height (around 20-30% or more) they may have lost the ability for the facet joints (located at the rear of the vertebrae) to be able tolerate end range extension as they collide together. This can then lead to irritation and inflammation in the facet joints, which will now make the person extension intolerant.

This is again where a thorough and individual assessment can help solve the problem. With methodical testing, we may find the person cannot tolerate any extension based work to heal their disc, or may we may find that a regressed position from the full cobra to one that has a less aggressive degree of extension may be beneficial.
Causes of Sciatica
Sciatica is a condition characterized by pain that radiates from the lower back through the buttocks, down the legs and can even reach into the toes. It occurs when the sciatic nerve, which is the longest nerve in the body, becomes compressed or irritated. The most common causes of sciatica include disc bulges, disc herniations, spinal stenosis, and spondylolisthesis.
But it is important to note that sciatica just means an impingement/compression on the sciatic nerve and there several different situations which can cause this. As such, sciatica should be seen as a collection of different mechanisms that create the same symptoms.

The first step in any case of sciatica is, of course, to get clarity on its exact mechanics in that person.
Is it discogenic (bulge / herniation) in nature? Is it a stenosis? Is it facet joint arthropathy? Is due to joint laxity? Is it due to compression from the ligaments or vascular system in the area? It can even be muscular in nature (piriformis syndrome).
We should also note that the age of the person can also predispose them more to certain types of sciatica. As we age (60+), our discs will naturally dehydrate and become less prone to developing disc bulges and herniations. However we will be more prone to stenosis from arthritic sources or from the hypertrophy of the ligaments
One very useful tool that we can use to diagnose the root cause is the Slump Test. This involves the patient sitting on a firm chair/bench with feet planted on the floor.

The are then instructed slip into a “slouched” or flexed position with their posture and observe any change in their pain levels.
The next stage is to apply some compression to the position by pulling themselves into the chair/bench. If their sciatic pain is stimulated or made worse, we know we have a discogenic aspect to their sciatic pain as compressed flexion has increased their symptoms.

We then return the patient to a more upright/neutral posture and ask them to repeat the addition of compression. If the pain is less than the flexed position we have confirmed that flexion is an aggravator to their injury.
However With facet joint arthropathy based sciatica, we may find the opposite to be true. In that flexion will alleviate the sciatic symptoms and lumbar extension will make it worse.
Again the goal with sciatica is to get a clear and precise diagnosis on the mechanics behind the pain. A disc bulge based sciatica must approached in a completely different way to an extension based sciatica.
Causes of End Plate Fractures
End plate fractures occur when the bony end plates of the vertebrae crack or break. The most common causes of end plate fractures include compression due to trauma or repetitive motion, osteoporosis, or tumors.

source: “Finite element investigation osteoporotic lumbar L1 vertebra buckling in a presence of torsional load”, Chaabarova et al.


End plates sit at the junction between the vertebrae and the discs at either end, knitting the two together and is the reason why discs cannot “slip”.
Brian’s Note: End-plates are tough! In fact when major a major spinal surgery takes place that requires the seperation of the disc from the vertebrae, the end-plate will need to be chiseled away from the bone.
In those who who weight train regularly (or lift heavy, repetitive loads due to their job), the a common issue is of an end-plate failure, whereby the spine has not been able to keep up the recovery demands and damage caused to the bony scaffolding that supports the end plate. Which in turn deteriorates, allowing the end-plate to fracture and fluid from the disc nucleus to leak into the vertebra. This usually accompanied by an audible “pop” sound at the moment of fracture and a deep, tooth-ache like pain in the spine afterwards.
These athletes will be highly sensitive to compressive loads until the end-plate has had time to heal.
Bone Callousing
The trabecular bone (the scaffolding) that sits beneath the end plate is broken down with micro-fractures during tasks that require repeated, heavy lifting and compression in the spine. With enough time between exposure (roughly 3-4 days), the process of bone callusing will allow that scaffolding to heal and become even stronger than the original, virgin bone.
This can be an important tool to help strength athletes be able to not only recover from an end plate fracture but to also allow the spine to adapt well enough to prevent future injury.
Brian’s Note: It also important to note that successful strength athletes will also further respect the healing process by also scheduling their training cycles with a de-load phase every 3-6 weeks.

Causes of Stenosis
Stenosis is a condition characterized by a narrowing of the spinal canal or intervertebral foramen, which can cause compression of the spinal nerves. The most common causes of stenosis include age-related changes (ligament hypertrophy, vascular claudication), arthritis, and tumors.
We have two main categories of stenosis:
1. Foraminal stenosis – stenosis that affects the lateral openings of the spinal canal.
2. Central Canal Stenosis – stenosis that affects the spinal canal itself.
Foraminal Stenosis


“The foramina, or openings, are present between every pair of vertebrae in these areas. A number of structures pass through the foramen. These are the root of each spinal nerve, the spinal artery of the segmental artery, communicating veins between the internal and external plexuses, recurrent meningeal (sinu-vertebral) nerves, and transforaminal ligaments.” – Wikipedia.
Central Canal Stenosis


It is important to note that stenosis can present as sciatica, whereby the the stenotic tissue can impinge upon the sciatic nerve giving pain or numbness down the leg and even into the toes.
Effects of Stenosis
Classically this will result in a diminishment of movement capacity, especially for walking; where even after a short period of time, sciatic like symptoms may present and/or worsen. It is generally more prevalent in the older age groups (60+); as stenosis is more likely due to the age accumulated arthritis combined with the increased likely hood of ligament hypertrophy and vascular claudication which will further diminish the shared space in the foramen and spinal canal.
Patients often get recommended to flex their lumbar spines to open up space around the nerves in the foramen, but for some this can actually exacerbate symptoms.
Instead, the “Park Bench Decompression” method developed by Prof. Stuart McGill can be a superb tool to use to alleviate symptoms and regain movement capacity, but again this will not work for everyone, so care must be taken in its application.
What is Spondylosis?
Spondylosis is an arthritic degeneration of the spine caused by wear and tear, usually found in older populations.
It can be used as bit of general term that encompasses “degenerative disease”, but care must be take to distinguish the type of mechanical problem and pain it is causing.
For example, a loss of disc height might result in facet joint irritation for some. For others, the arthritis may be causing a stenosis issue that impinges upon the sciatic nerve.

What Causes Spondylolysis?
Spondylolysis is considered to be a fracture (with no slippage of the vertebra) that results from mechanical stress at the pars interarticularis. Generally these stress fractures occur due to repeated end-range movements, but can also be caused by severe trauma.
If left untreated, a spondylolysis can then progress into spondylolisthesis (fracture with forward slippage of the vertebra)
Brian’s Note: A simple visual cue here is to imagine a repeatedly folding a credit card backwards and forwards until it snaps. Repeated end range movements place force on the pars interarticularis, with enough exposure and minimal rest in between, the bone can fracture.


What Causes Spondylolisthesis?
Spondylolisthesis is considered to be the forward slippage of the vertebra in relation to the vertebra below it.

There are 6 Different Types or Causes of Spondylolisthesis:
| Spondylolisthesis Type | Cause |
| 1. Dysplastic | Congenital abnormalities where the bones of the spine do not form completely during pregnancy. |
| 2. Isthmic | Stress fractures in the pars interarticularis from repeated end range stress |
| 3. Degenerative | Age related degeneration – particularly in the facet joints |
| 4. Traumatic | Acute fractures after severe trauma (car accidents, etc) |
| 5. Pathological | Bone diseases, tumours and infections |
| 6. Iatrogenic | A result from previous surgical intervention – usually a decompression or facetectomy type of procedure carried out without further stabilisation to the area. |
Isthmic Spondylolisthesis
Young gymnasts and cricket fast bowlers are especially prone to this type of injury due the nature of repeated end range extension required during the participation of their sport. The injury will first progress from a spondylolysis (fracture with no slippage).
As such, the most prudent form of action is to stop the activity causing the damage. Many young athletes will struggle with this, but if given enough recovery, the fracture will heal. If, however, the aggravating activity continues, the injury may then progress into full blown spondylolisthesis where the damaged vertebra will begin to slip away from the vertebra below it.
Muscular Imbalance and Inhibition
Often a contentious issue among practitioners of different disciplines, the issue of muscular imbalance and inhibition now has a growing pool of evidence to support its existence and its underlying mechanisms.
Gluteal Amnesia
Probably the most common issue and one that seen as a contributing factor to muscular pain in lower back injuries, is that of gluteal amnesia.
The mechanism behind the issue of “lazy glutes” is that of arthrogenic neuromuscular inhibition (AMI). Which is a reflex inhibition of musculature surrounding a joint after distension or damage to that joint.
Those familiar with the work of Prof. Stuart McGill on this topic will be aware of a study carried out by him and his team on measuring gluteal amnesia in real time.
They began by take base measurements of glute activity by having study participants perform glute bridge exercises. They then performed a procedure called “capsular distension arthrogram” to create pain in the hip joint. When retesting the bridge after this procedure, the activity of the glute max on the side of the painful hip was found to be significantly reduced.
The idea is not that the glutes are “switched off” completely, but rather the brain has diminished neural drive to the glutes in response to the pain created at the joint.

It is thought that AMI is a contributing factor in the corruption of neural engrams, whereby engrained movement and posture habits become corrupted and develop mistakes in response to the pain of injury. As such, this would suggest an appropriate response to situations the involve a corruption of movement engrams would be that of a “re-learning” or re-education of those movement engrams to develop movement patterns that spare the back from pain.
Muscular Recruitment Patterns and Posture
The role and affects of day-to-day posture habits on muscular atrophy, recruitment and strength are now also well understood.
An example of this is that of multifidus weakness/atrophy and those with recurrent low back pain.
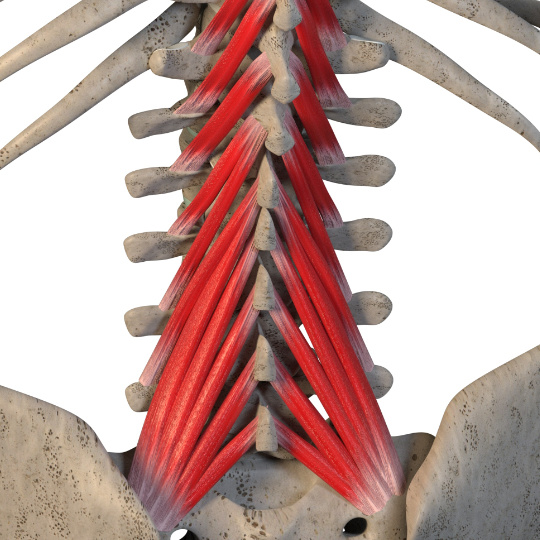

Multifidus plays an important role in spinal stability, think of it has a series of guy-wires that helps stabilise and provide movement for individual sections of the spine. In particular it helps with extension and rotational movement of the spine.
In those with chronic lower back pain, it has been observed that the multifidus muscle has atrophied with fatty tissue replacement. When atrophy has occurred, multifidus has reduced ability to aid in these critical functions that help stabilize the spine.
Treatment plans that have facilitated the hypertrophy of multifidus have shown a correlation in a reduction in lower back pain.
So although multifidus strengthening and hypertrophy on its own is not a panacea for lower back pain, it can ben an important piece of the puzzle when forming a complete solution to chronic lower back pain.
Exercises that help challenge multifidus for hypertrophy and strength include those that challenge extension and rotation at the same time. A good example of this is the Bird-Dog exercise and its variations.

Summary
The scope of this article was not to provide an exhaustive list of lower back pain causes and potential solutions, but rather highlight some of the most common issues that can successfully tested for and identified; with each having their own particular characteristics, treatment indications and contraindications.
The goal with this article was to present a mere “dipping of the toe” into the area of lower back pain in the hopes that it will give an idea of the possible and various sources of a patient’s back pain; while also demonstrating the inherent laziness of the “Non-Specific Lower Back Pain” (NSLBP) label that often gets placed on difficult back pain cases.
A good practitioner/clinician will be able to clearly diagnose the cause of a patient’s pain by methodical investigation of the patient’s injury type, history, day-to-day movement habits, provocation and muscular tests.
References and Further Reading:
Scannell, J. P., & McGill, S. (2009). Disc prolapse: Evidence of reversal with repeated extension. Spine. https://doi.org/10.1097/BRS.0b013e31819712a6
Tampier, C., Drake, J., Callaghan, J., & McGill, S. (2007). Progressive disc herniation: An investigation of the mechanism using radiologic, histochemical, and microscopic dissection techniques on a porcine model. Spine. https://doi.org/10.1097/BRS.0b013e31815b64f5
Bogduk, N., Aprill, C., & Derby, R. (2013). Lumbar discogenic pain: State-of-the-art review. Pain Med. https://doi.org/10.1111/pme.12082
Benson, R. B., Tavares, S., Robertson, S., Sharp, R., & Marshall, R. (2010). Conservatively treated massive prolapsed discs: A 7-year follow-up. Ann R Coll Surg Engl. https://doi.org/10.1308/003588410X12518836438840
Chabarova, O., Alekna, V., KaÄianauskas, R., & Ardatov, O. (2017). Finite element investigation osteoporotic lumbar L1 vertebra buckling in a presence of torsional load. MECHANIKA. https://doi.org/10.5755/J01.MECH.23.3.18476
Zhang, S. (2021). Image classification of osteoporotic vertebral fracture with endplate-disc complex Injury. BMC Musculoskeletal Disorders, (22).
Syrmou, E., Et al (2010). Spondylolysis: A review and reappraisal. Hippokratia. https://doi.org/PMCID: PMC2843565
Buckthorpe, M., Et al (2019). ASSESSING AND TREATING GLUTEUS MAXIMUS WEAKNESS – A CLINICAL COMMENTARY. Int J Sports Phys Ther. https://doi.org/PMCID: PMC6670060
Freeman S, Mascia A, McGill SM. Arthrogenic neuromuscular inhibition: a foundational investigation of existence in the hip joint. Clin Biomech. 2013; 28:171-77.
Bullock-Saxton JE, Janda V, Bullock MI. Reflex activation of gluteal muscles in walking. An approach to restoration of muscle function for patients with low-back pain. Spine. 1993;18(6):704-8
Nelson-Wong E, Alex B, Csepe D, Lancaster D, Callaghan JP. Altered muscle recruitment during extension from trunk flexion in low back pain developers. Clin Biomech. 2012;27(10):994-8
Olfat M, Perry J, Hislop H. Relationship between wire EMG activity, muscle length, and torque of the hamstrings. Clin Biomec. 2002;17(8):569-579
Freeman, M. (2010). The Role of the Lumbar Multifidus in Chronic Low Back Pain: A Review. PM&R, 2(2). https://doi.org/10.1016/j.pmrj.2009.11.006
Hodges, P, et al. (2019). Changes in Structure and Function of the Back Muscles in Low Back Pain: Different Time Points, Observations, and Mechanisms. Journal of Orthopaedic & Sports Physical Therapy, 49(6). https://doi.org/https://www.jospt.org/doi/10.2519/jospt.2019.8827
Woodham, M., et al (2014). Long-Term Lumbar Multifidus Muscle Atrophy Changes Documented With Magnetic Resonance Imaging: A Case Series. British Journal of Sports Medicine. https://doi.org/10.3941/jrcr.v8i5.1401
Daneels, L., et al (2001). Effects of three different training modalities on the cross sectional area of the lumbar multifidus muscle in patients with chronic low back pain. British Journal of Sports Medicine.
Faur, C., et al (2019). Correlation between multifidus fatty atrophy and lumbar disc degeneration in low back pain. BMC Musculoskeletal Disorders.
Hodges, P, et al (2021). Effect of low back pain on the muscles controlling the sitting posture. J Phys Ther Sci. https://doi.org/10.1589/jpts.33.295
McGill, S. (2015). Low Back Disorders: Evidence-Based Prevention and Rehabilitation (3rd ed.)
McGill, S. 2003, Spine flexion exercise: Myths, Truths and Issues affecting health and performance
https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/musculoskeletal-conditions/contents/back-pain-and-problems
https://www.aihw.gov.au/getmedia/0d9f8959-2a1c-4c99-8c7e-0c8a878f4d6c/Back%20problems.pdf.aspx